Table of contents
- The Intricate Connection: Unraveling Diabetes and Chronic Pain
- The Art of Managing Chronic Pain in Diabetes
- The Power of Healthy Eating for Diabetes and Chronic Pain
- The Ultimate Guide to Pain Management in Diabetes
Diabetes, a chronic disease affecting millions worldwide, is not only associated with high blood sugar levels but also with another troublesome symptom: chronic pain. This article explores the intricate relationship between diabetes and chronic pain, delving into the potential causes, risk factors, and effective management strategies for individuals living with both conditions. Understanding this connection is crucial in improving the quality of life for those affected by diabetes and chronic pain.
The Intricate Connection: Unraveling Diabetes and Chronic Pain
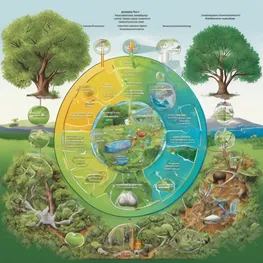
High blood sugar levels can have detrimental effects on the body, particularly on the nerves, leading to nerve damage and chronic pain. Understanding the intricate connection between diabetes and chronic pain is crucial for managing these conditions effectively.
- Elevated blood sugar levels can cause damage to the nerves throughout the body. The excess glucose can disrupt the normal functioning of the nerves, leading to their deterioration over time.
- Nerve damage, known as diabetic neuropathy, is a common complication of diabetes. It primarily affects the peripheral nerves, which transmit sensory information from the body to the brain. As the nerves become damaged, they may send abnormal signals or fail to transmit signals altogether, resulting in chronic pain.
- High blood sugar levels can also impair blood flow to the nerves, further exacerbating nerve damage and pain. The reduced blood supply restricts the delivery of essential nutrients and oxygen to the nerves, hindering their ability to heal and regenerate.
- Chronic pain associated with diabetic neuropathy can manifest in various ways, including sharp or shooting pain, tingling or numbness, and sensitivity to touch. The severity of the pain can vary from mild discomfort to debilitating agony, significantly impairing the individual's quality of life.
- Managing blood sugar levels through proper diabetes management is essential for preventing and reducing nerve damage and chronic pain. Regular monitoring of blood glucose levels, maintaining a balanced diet, engaging in regular physical activity, and taking prescribed medications can help control blood sugar and minimize the risk of complications.
- Additionally, treatments for chronic pain resulting from nerve damage may include medications to alleviate pain, physical therapy to improve nerve function, and lifestyle modifications to reduce further nerve damage.
The Art of Managing Chronic Pain in Diabetes
Managing chronic pain is essential for individuals with diabetes. By incorporating regular exercise and stress reduction techniques into their daily routine, patients can effectively manage their pain and improve their overall quality of life.
-
Regular Exercise
Engaging in regular exercise has numerous benefits for individuals with chronic pain. Exercise helps to improve circulation, strengthen muscles, and increase flexibility. It also releases endorphins, which are natural pain relievers. Incorporating activities such as walking, swimming, and yoga into a daily routine can help alleviate pain and improve mobility.
-
Stress Reduction Techniques
Stress has a significant impact on chronic pain. High levels of stress can exacerbate pain symptoms and make it more difficult to manage. Incorporating stress reduction techniques such as deep breathing exercises, meditation, and mindfulness can help to reduce stress levels and promote relaxation. This, in turn, can reduce pain levels and improve overall well-being.
The Power of Healthy Eating for Diabetes and Chronic Pain
For individuals managing blood sugar levels and chronic pain, a balanced diet plays a crucial role. Including whole grains, fruits, vegetables, and lean proteins can provide essential nutrients while maintaining stable blood sugar levels. Whole grains like quinoa and brown rice offer fiber and slow-release carbohydrates, preventing spikes in blood sugar. Fruits and vegetables contribute vitamins, minerals, and antioxidants that promote overall health. Lean proteins such as chicken breast and legumes provide necessary protein without excessive fat. By adopting a balanced diet rich in these foods, individuals can effectively manage blood sugar levels and reduce chronic pain.
The Ultimate Guide to Pain Management in Diabetes
In the Ultimate Guide to Pain Management in Diabetes, we offer expert advice on complementary therapies and alternative treatments for reducing chronic pain. Living with diabetes can be challenging, and chronic pain adds an additional burden. We understand that traditional treatments may not always be effective, so we explore a range of complementary therapies such as acupuncture, massage therapy, and herbal remedies. Additionally, we provide information on alternative treatments like meditation, yoga, and biofeedback. With our comprehensive guide, individuals with diabetes can explore these options to find relief from chronic pain and improve their quality of life.
In conclusion, it is evident that there is a strong relationship between diabetes and chronic pain. Diabetic neuropathy, which affects a significant number of individuals with diabetes, can cause persistent pain and discomfort. Moreover, the complex interplay between inflammation, nerve damage, and glucose control in diabetes contributes to the development and persistence of chronic pain. Recognizing this connection is crucial for healthcare professionals to provide targeted treatment options and support for patients living with both conditions. Further research is needed to better understand the mechanisms involved and develop more effective interventions for managing diabetes-related chronic pain.
Frequently asked questions related to relationship between diabetes and chronic pain
How does diabetes contribute to chronic pain?
Diabetes can lead to nerve damage, which can cause chronic pain. High blood sugar levels can damage the nerves over time, leading to a condition known as diabetic neuropathy. This can result in pain, tingling, and numbness in the affected areas.
Can managing diabetes help reduce chronic pain?
Yes, managing diabetes effectively can help reduce chronic pain. Keeping blood sugar levels within the target range can help prevent or delay the onset of diabetic neuropathy and minimize its symptoms. This can be achieved through lifestyle changes, medication, and regular monitoring.
What treatment options are available for diabetic neuropathy?
Treatment for diabetic neuropathy focuses on managing the symptoms and preventing further nerve damage. This may include pain medications, antidepressants, anticonvulsants, topical treatments, physical therapy, and lifestyle modifications such as regular exercise and a healthy diet.
Can chronic pain be a warning sign of undiagnosed diabetes?
Yes, chronic pain can be a warning sign of undiagnosed diabetes. If you are experiencing persistent or unexplained pain, especially in the extremities, it is important to consult a healthcare professional for a proper evaluation and diagnosis.
What are the common symptoms of diabetic neuropathy?
The symptoms of diabetic neuropathy include pain or discomfort in the feet, legs, hands, or arms; tingling or numbness in the affected areas; sensitivity to touch; muscle weakness; and problems with coordination and balance.
Are there different types of diabetic neuropathy?
Yes, there are several types of diabetic neuropathy. The most common type is peripheral neuropathy, which affects the feet, legs, hands, and arms. Other types include autonomic neuropathy, focal neuropathy, and proximal neuropathy.