The Impact of Diabetes on Bone Density and Osteoporosis
Discover how diabetes affects bone density and increases the risk of osteoporosis, uncovering the lesser-known consequences of this chronic condition.
Discover how diabetes affects bone density and increases the risk of osteoporosis, uncovering the lesser-known consequences of this chronic condition.
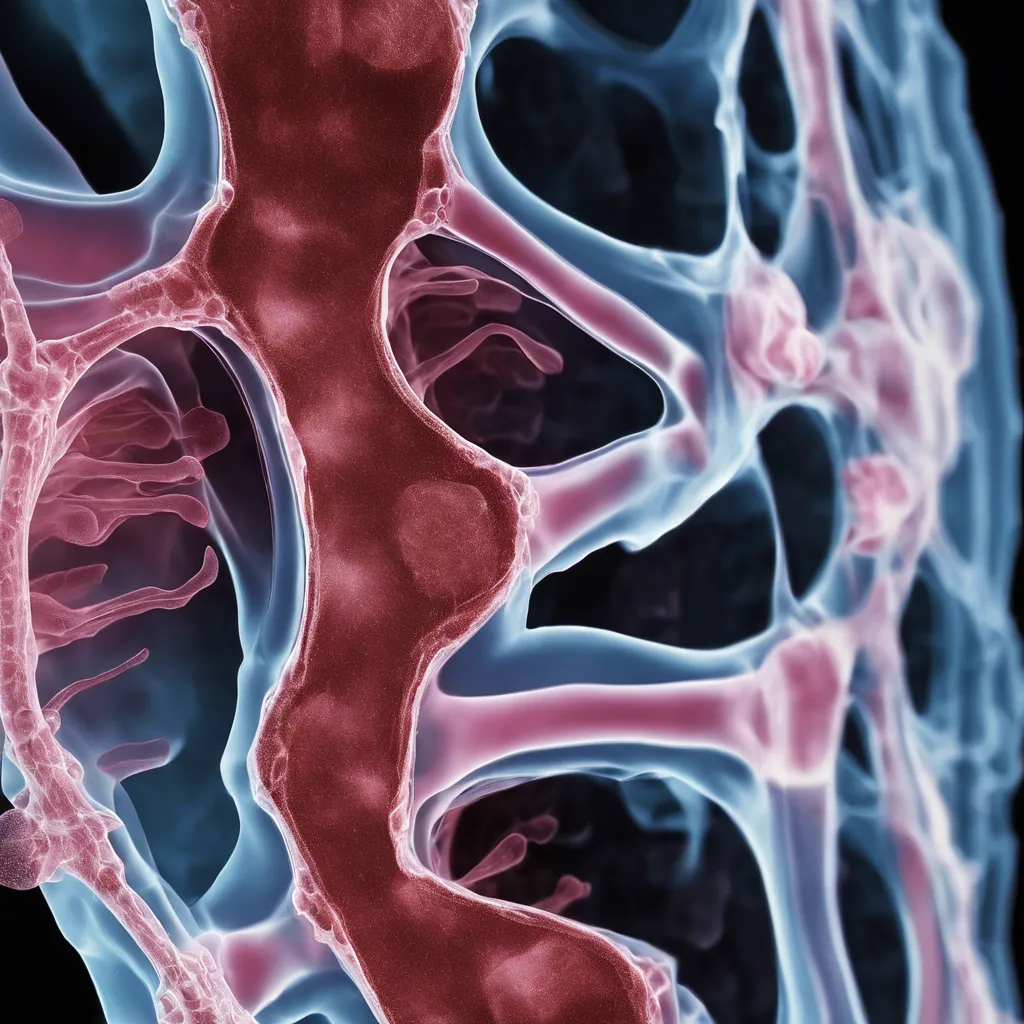
Diabetes is a prevalent chronic condition affecting millions worldwide, and its effects extend beyond blood sugar regulation. Recent research suggests that diabetes can have a significant impact on bone health, leading to decreased bone density and an increased risk of osteoporosis. This article delves into the intricate relationship between diabetes and bone health, exploring the underlying mechanisms, risk factors, and potential interventions to mitigate the detrimental effects.
Diabetes and Bone Density: Decoding the Complex Relationship
Having diabetes can significantly increase the risk of developing osteoporosis, a condition characterized by weak and brittle bones. The mechanisms behind this link involve factors such as hormonal imbalances, inflammation, and impaired bone formation and repair.
Maintaining stable blood sugar levels can help preserve bone density.
Diabetes has been shown to have negative effects on bone health. Individuals with diabetes are more susceptible to developing osteoporosis and experiencing bone fractures. This is due in part to the damage that high blood sugar levels can cause to the bone structure and the impaired ability of the body to effectively repair and regenerate bones.
Stable blood sugar levels are crucial for overall health, including bone health. When blood sugar levels are excessively high, it can lead to chronic inflammation and oxidative stress, which can have detrimental effects on bone density. Conversely, low blood sugar levels can lead to decreased bone density and an increased risk of fractures.
Maintaining stable blood sugar levels helps preserve bone density by reducing the negative impact of diabetes on bone health. By controlling blood sugar levels through lifestyle modifications or medication, individuals with diabetes can minimize the damage to their bones, promote bone healing and regeneration, and reduce the risk of osteoporosis and bone fractures.
To maintain stable blood sugar levels, individuals with diabetes should focus on adopting a balanced and nutritious diet, engaging in regular exercise, managing stress levels, and taking prescribed medications as directed. Monitoring blood sugar levels regularly and working closely with healthcare professionals can also help in maintaining stable blood sugar levels and optimizing bone health.
One key tip for successfully managing diabetes and promoting strong and healthy bones is to work closely with your healthcare team to effectively manage blood sugar levels. Regular communication with your healthcare team can help ensure that your treatment plan is tailored to your specific needs and goals, leading to better overall diabetes management and bone health.
In conclusion, it is evident that diabetes has a significant impact on bone density and increases the risk of developing osteoporosis. The chronic hyperglycemic state in diabetes negatively affects bone metabolism, leading to reduced bone mineral density and an increased risk of fractures. Furthermore, the underlying mechanisms, including insulin deficiency or resistance, inflammation, oxidative stress, and advanced glycation end-products, further contribute to bone loss in individuals with diabetes. Understanding these interactions is crucial for early detection and intervention strategies to minimize the risk of osteoporosis in diabetic patients and improve their overall bone health. Further research is needed to explore effective preventive and treatment measures tailored specifically for this population.
Diabetes can affect bone density by disrupting the normal balance between bone formation and resorption. High blood sugar levels can lead to a decrease in bone mineral density, making the bones more fragile and prone to fractures.
Individuals with diabetes and osteoporosis should follow a well-balanced diet that includes foods rich in calcium and vitamin D, such as dairy products, leafy greens, fortified cereals, and fatty fish. It is also important to monitor carbohydrate intake to maintain stable blood sugar levels.
Some diabetes medications, such as thiazolidinediones, have been linked to an increased risk of bone fractures. However, other diabetes medications, like metformin, may actually have a protective effect on bone health. It is important for individuals with diabetes to discuss their medication regimen with their healthcare provider to determine any potential impact on bone health.
Several lifestyle changes can improve bone health in individuals with diabetes. These include engaging in weight-bearing exercises, consuming a balanced diet rich in calcium and vitamin D, quitting smoking, limiting alcohol intake, and managing blood sugar levels effectively through proper diabetes management.
Yes, diabetes increases the risk of developing osteoporosis. The chronic inflammation and elevated blood sugar levels associated with diabetes can negatively affect bone health, leading to a higher risk of osteoporosis.
To prevent bone fractures, individuals with diabetes should take steps to maintain good bone health. This includes participating in weight-bearing exercises, practicing good balance and posture, avoiding falls, wearing appropriate footwear, and discussing bone health concerns with their healthcare provider.